Intermittent versus continuous androgen deprivation in prostate cancer.

Abstract
BACKGROUND:
Castration resistance occurs in most patients with metastatic hormone-sensitive prostate cancer who are receiving androgen–deprivation therapy. Replacing androgens before progression of the disease is hypothesized to prolong androgen dependence.
METHODS:
Men with newly diagnosed, metastatic, hormone-sensitive prostate cancer, a performance status of 0 to 2, and a prostate-specific antigen (PSA) level of 5 ng per milliliter or higher received a luteinizing hormone-releasing hormone analogue and an antiandrogen agent for 7 months. We then randomly assigned patients in whom the PSA level fell to 4 ng per milliliter or lower to continuous or intermittent androgen deprivation, with patients stratified according to prior or no prior hormonal therapy, performance status, and extent of disease (minimal or extensive). The coprimary objectives were to assess whether intermittent therapy was noninferior to continuous therapy with respect to survival, with a one-sided test with an upper boundary of the hazard ratio of 1.20, and whether quality of life differed between the groups 3 months after randomization.
RESULTS:
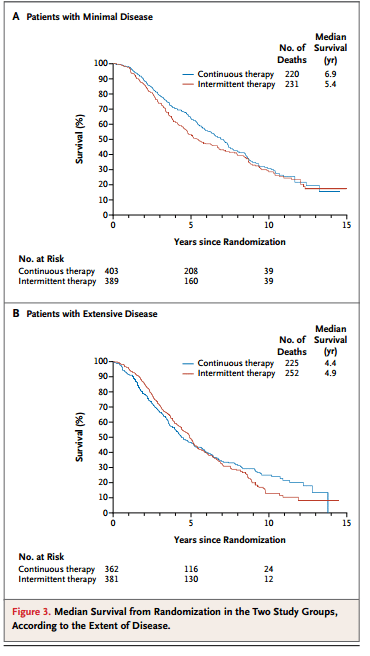
A total of 3040 patients were enrolled, of whom 1535 were included in the analysis: 765 randomly assigned to continuous androgen deprivation and 770 assigned to intermittent androgen deprivation. The median follow-up period was 9.8 years. Median survival was 5.8 years in the continuous-therapy group and 5.1 years in the intermittent-therapy group (hazard ratio for death with intermittent therapy, 1.10; 90% confidence interval, 0.99 to 1.23). Intermittent therapy was associated with better erectile function and mental health (P<0.001 and P=0.003, respectively) at month 3 but not thereafter. There were no significant differences between the groups in the number of treatment-related high-grade adverse events.
CONCLUSIONS:
Our findings were statistically inconclusive. In patients with metastatic hormone-sensitive prostate cancer, the confidence interval for survival exceeded the upper boundary for noninferiority, suggesting that we cannot rule out a 20% greater risk of death with intermittent therapy than with continuous therapy, but too few events occurred to rule out significant inferiority of intermittent therapy. Intermittent therapy resulted in small improvements in quality of life. (Funded by the National Cancer Institute and others; ClinicalTrials.gov number, NCT00002651.).