Diagnosis
There are numerous methods of detecting and diagnosing prostate cancer:
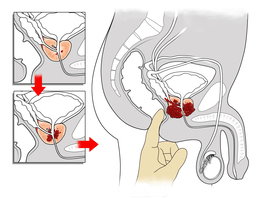
- Digital Rectal Exam (DRE) – The doctor gently inserts a lubricated, gloved finger into the rectum to check for growths and an enlargement of the prostate gland.
- Prostate-Specific Antigen (PSA) Test – PSA is a protein produced by the prostate gland that is released into the bloodstream in small amounts, and is detected via blood tests. If the PSA amount within the blood is higher than normal, prostate cancer is likely present.
- Prostate Cancer Antigen 3 (PCA3) Test – This test is conducted via a urine sample to detect PCA3, a gene that is over expressed in prostate cancer cells. Its presence in urine indicates the existence of prostate cancer.
- Percent-Free PSA Ratio – This blood test measures the amount of PSA that circulates individually (unbound) in the blood, as well as the amount that is bound with other blood proteins. If PSA results are elevated and the percent-free ratio is low, prostate cancer is likely to be present.
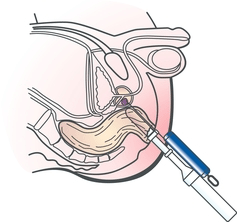
- Ultrasound – A transrectal ultrasound provides an image that can be used to determine the size of the prostate gland and detect suspicious tissue.
- Biopsy– A prostate biopsy involves removing small amounts of tissue to examine under a microscope, which allows doctors to determine whether cancer is present.
Treatment
Several treatment options are available for prostate cancer patients. The standard therapies for men with organ-confined, or localized, prostate cancer include:
- Active Surveillance – Conducting regular digital rectal examinations, PSA tests and repeat prostate biopsies is a treatment option if prostate cancer is not causing symptoms and anticipated to grow slowly.
- Surgery (Prostatectomy) – Surgical treatment involves removing the prostate gland and seminal vesicles and in some cases sampling lymph nodes in the pelvis.
- Radiation Therapy – During radiation treatment, high energy X-Ray waves are targeted at cancerous tumors resulting in damage to the DNA of the cells, leading to death of the cancer cells.
- External Beam Radiotherapy – X-ray beams are passed through the body from the outside (like a Chest Xray), aimed at the prostate gland, in small doses over many days.
- Brachytherapy – Radioactive seeds/pellets are implanted in the prostate gland and give off radiation over many days to the prostate gland.
Other treatment options include:
- Hormonal Therapy – Most prostate cancer cells are dependent upon testosterone (male hormone) for growth. Hormonal therapy for prostate cancer involves removing or blocking the effects of testosterone and its stimulating effect on prostate cancer cells.
- Cryotherapy – Cryotherapy is a relatively new form of treatment that uses controlled freeze and thaw cycles to destroy prostate cancer cells.
- Chemotherapy – Typically is used to treat advanced, castrate resistant disease, chemotherapy is a systematic treatment that uses anticancer medication to destroy cancer cells.
To learn about other available treatment options, talk with your doctor.
For more information please visit the Prostate Cancer Canada website.